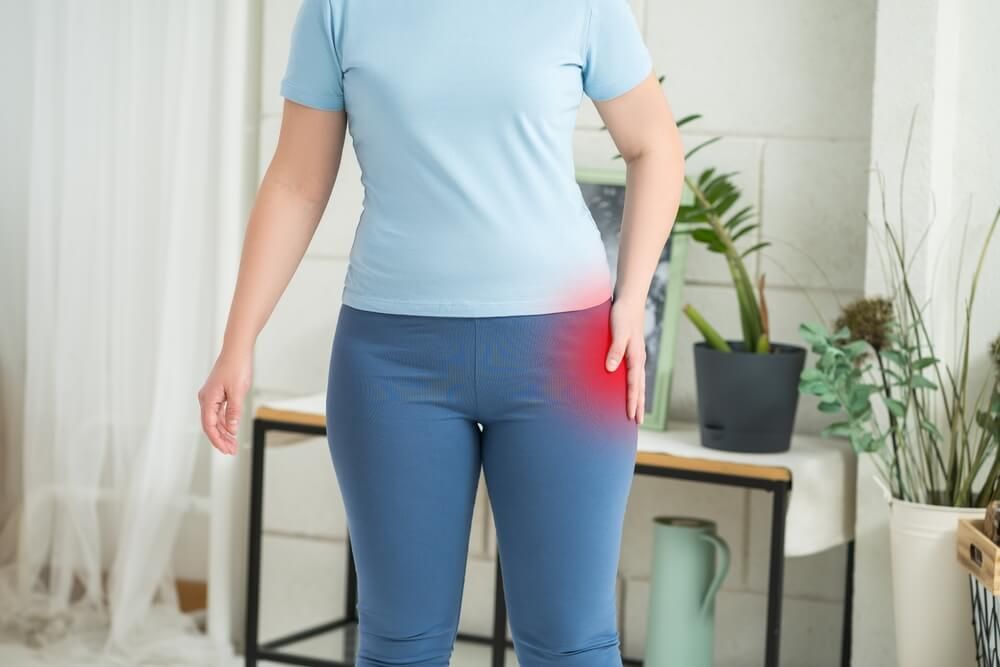
Hip bursitis is a painful condition that affects the small fluid-filled sacs—called bursae—located near the hip joint. These sacs serve to cushion the muscles, tendons, and bones, reducing friction during movement. When one of the major bursae in the hip becomes inflamed, typically the trochanteric bursa or iliopsoas bursa, it can result in sharp or aching pain around the outer or front side of the hip. This discomfort often worsens with movement, pressure, or prolonged periods of standing or sitting.
The condition can develop from repetitive motion, overuse, trauma, poor posture, or even underlying biomechanical issues such as leg length discrepancy or gait abnormalities. It is also more common in middle-aged or older adults, especially women. Despite being non-arthritic in nature, hip bursitis can significantly impair a person’s mobility and daily activities. Fortunately, targeted therapies offer effective, non-surgical solutions to control pain and restore function.
Recognizing Symptoms and Getting Diagnosed
The hallmark symptom of hip bursitis is localized pain, which is most commonly felt over the outside of the hip and may radiate down the thigh. The pain may be sharp and intense during physical activity or when lying on the affected side, and it often becomes a dull ache that persists through the day. Swelling, tenderness, and increased sensitivity to touch in the hip region are also common signs. Some individuals may experience stiffness or a snapping sensation when moving the hip joint.
To properly diagnose hip bursitis, physicians begin with a physical examination, asking patients about their symptoms, activity levels, and medical history. Imaging studies such as X-rays or MRIs may be used to rule out other causes of hip pain, including arthritis or tendon injuries. In some cases, ultrasound-guided injections may be used both to diagnose and treat the affected bursa, helping to confirm the location of inflammation.
Non-Surgical Treatment Strategies
For most patients, hip bursitis responds well to conservative, non-invasive treatments. Rest and activity modification are often the first steps in reducing irritation of the bursa. Patients may be advised to avoid repetitive hip motions, minimize extended periods of standing, or refrain from sleeping on the affected side. Ice therapy can also help reduce inflammation and alleviate acute pain.
Anti-inflammatory medications, such as NSAIDs (non-steroidal anti-inflammatory drugs), are commonly prescribed to manage symptoms. In some cases, corticosteroid injections may be administered directly into the bursa to provide targeted relief. These injections are particularly effective in decreasing inflammation and pain in cases where oral medications are insufficient. When used judiciously, these targeted therapies can provide long-term relief with minimal side effects.
Physical Therapy and Stretching
Physical therapy is a central component of a comprehensive treatment plan for hip bursitis. A licensed therapist will tailor an exercise program to improve flexibility, strengthen surrounding muscles, and correct any postural imbalances contributing to joint stress. Emphasis is often placed on the gluteal muscles and hip stabilizers, which can alleviate pressure on the bursa and improve gait mechanics.
Stretching routines are also important, especially for the iliotibial band and hip flexors, which are frequently tight in patients with bursitis. Therapists may incorporate modalities such as ultrasound, soft tissue massage, and electrical stimulation to further reduce inflammation and promote healing. The goal is to restore mobility without re-aggravating the bursa.
Advanced Therapeutic Interventions
For patients who do not respond to initial conservative treatments, targeted therapies such as image-guided corticosteroid injections can offer precise relief. Using ultrasound or fluoroscopy, a physician can deliver medication directly to the inflamed bursa, often providing quick and significant symptom improvement. These injections can be repeated as needed, though typically no more than a few times per year to avoid tissue weakening.
Emerging regenerative therapies, such as platelet-rich plasma (PRP) injections, are also being explored for their ability to reduce inflammation and support tissue healing. PRP is derived from the patient’s own blood and contains growth factors that may promote recovery in chronic or stubborn cases of bursitis. While research is ongoing, early results suggest this may be a valuable tool for those seeking alternatives to corticosteroids.
Addressing Underlying Biomechanical Issues
Another key aspect of long-term recovery is addressing the root causes of hip bursitis. This may involve evaluating and correcting issues such as leg length discrepancies, abnormal gait patterns, or improper footwear. Custom orthotics, shoe inserts, and changes in walking habits can all make a significant difference in relieving stress on the hip joint. In more complex cases, collaboration between physical therapists, orthopedic specialists, and podiatrists may be necessary to develop a fully integrative treatment plan.
Long-Term Management and Prevention
Managing hip bursitis successfully involves not just treating current symptoms but also preventing recurrence. Patients are often encouraged to maintain a regular stretching and strengthening routine even after symptoms have resolved. Monitoring activity levels and avoiding overuse are also essential for keeping the hip joint healthy.
Maintaining a healthy body weight can further reduce the mechanical load on the hip. For those who engage in sports or high-impact activities, cross-training and using proper body mechanics can significantly reduce the risk of future flare-ups. Education plays a vital role—patients who understand their condition are more empowered to make decisions that support long-term joint health and mobility.
At Premier Orthopaedics & Sports Medicine, P.C., with locations in Bloomfield, Englewood, and Union City, NJ, we specialize in helping patients find relief through personalized, evidence-based care. Whether you’re dealing with chronic hip pain or a recent flare-up, our team is here to support you with targeted therapies designed to restore movement and improve quality of life.
Sources
Strauss, E. J., Nho, S. J., Kelly, B. T., et al. (2010). Greater Trochanteric Pain Syndrome. Clinical Orthopaedics and Related Research.
Silva, F., & Adams, T. (2016). Trochanteric Bursitis: An Overlooked Cause of Hip Pain. Journal of the American Board of Family Medicine.
Collee, G., Dijkmans, B. A., Vandenbroucke, J. P., et al. (1991). Greater Trochanteric Pain Syndrome. Archives of Physical Medicine and Rehabilitation.